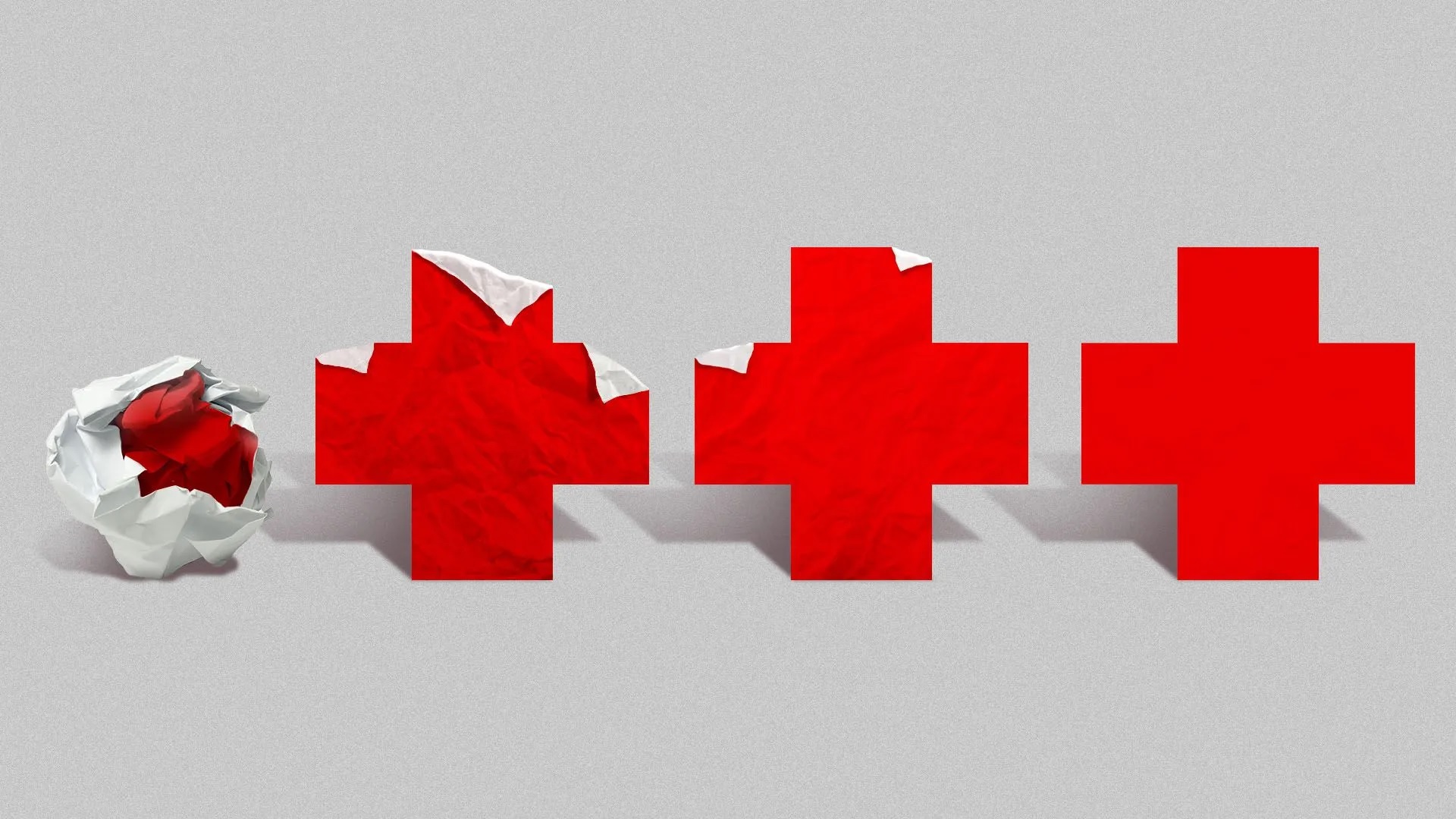
In the aftermath of pandemic protections expiring in April, nearly 4 million Americans have been removed from Medicaid, a number expected to reach 24 million. NPR’s Selena Simmons-Duffin explores this process where states are reevaluating Medicaid eligibility. The removals, often due to paperwork issues, have caused disruptions in healthcare access. Disenrollment rates vary significantly across states, from 82% in Texas to 8% in Wyoming. Translation challenges in communities like the Marshallese in Arkansas have compounded the issue. Displaced individuals are urged to explore reenrollment options or subsidized plans on healthcare.gov for continued coverage.
Millions of Americans are facing the challenge of navigating the complex terrain of Medicaid disenrollment due to shifting policies and expiring pandemic protections. It is crucial to understand the intricacies of this process, as nearly 4 million individuals have already been removed from Medicaid, and this number is expected to soar to 24 million. To help those affected, we have created a comprehensive guide that delves into the essential steps and crucial tips to adapt to these changes. Our guide covers everything from understanding the reasons behind disenrollment to exploring reenrollment options and subsidized plans. We provide valuable insights to ensure uninterrupted healthcare access for those affected.
LEILA FADEL, HOST:
Since the expiration of pandemic protections in April, nearly 4 million people nationwide have been removed from Medicaid, with projections indicating this number could surge to 24 million. NPR’s Selena Simmons-Duffin reports on the ongoing process as states reassess Medicaid eligibility.
SELENA SIMMONS-DUFFIN, BYLINE: Just months ago, in March, a staggering 93 million people were enrolled in Medicaid, representing a quarter of the country’s population, benefiting from the public health insurance program designed for those with limited incomes. The pandemic-era policy allowed new enrollments without displacing existing beneficiaries for three years, leading to a significant expansion. Now, states are undergoing what experts term “the great unwinding” – a return to the customary annual eligibility verification process.
JENNIFER TOLBERT: Seventy-four percent of individuals, on average, are losing coverage due to paperwork-related issues.
SIMMONS-DUFFIN: That’s Jennifer Tolbert, director of state health reform at KFF, explaining that many are losing coverage because of administrative challenges, such as not receiving renewal notices on time or encountering difficulties in submitting necessary documents.
TOLBERT: They didn’t get the renewal notice in time. They didn’t understand what they needed to do. Or they submitted the documents, but the state was unable to process those documents before their coverage was ended.
SIMMONS-DUFFIN: Tolbert notes that some wrongfully disenrolled individuals may swiftly reenroll, yet even a brief disruption in coverage can be highly disruptive, especially for those dealing with illness or struggling to access essential medications. Each state manages its Medicaid program, leading to significant variations in disenrollment rates.
TOLBERT: In Texas, during the initial phase of unwinding, they reported a disenrollment rate of 82%.
SIMMONS-DUFFIN: This is in stark contrast to Wyoming, where the disenrollment rate stands at 8%. Tolbert emphasizes that understanding the causes of these disparities requires more data. In some cases, like in Arkansas, complications arose due to translation issues within specific communities.
KEESA SMITH: The documents that DHS had translated into Marshallese did not make sense. The one thing that did translate was that these individuals had done something drastically wrong.
SIMMONS-DUFFIN: That’s Keesa Smith, a former employee of Arkansas’s Department of Human Services, highlighting challenges faced by the Marshallese community. For those affected by Medicaid disenrollment, experts and advocates urge individuals to explore alternative options. If the loss of coverage was due to paperwork errors, enrollment is possible. If eligibility criteria are no longer met, there are subsidized plans available on healthcare.gov, ensuring affordable monthly costs.
This evolving situation necessitates careful navigation, emphasizing the importance of staying informed about available resources and support networks. Selena Simmons-Duffin, NPR News.
