Research reveals that women’s heightened vulnerability to autoimmune disorders may stem from the intricate handling of the additional X chromosome in their bodies. The presence of two X chromosomes necessitates a mechanism to silence one, leading to the formation of protein clusters that have been linked to autoimmune diseases. By understanding these biological intricacies, scientists aim to develop better diagnostic tools and treatments for autoimmune disorders, potentially transforming patient care.
Women are disproportionately affected by autoimmune disorders compared to men, with approximately 80% of cases occurring in females. Recent research delves into the genetic underpinnings of this gender disparity, focusing on the handling of the X chromosome in female biology. The discovery of Xist-mediated protein clusters as potential triggers for autoimmune diseases offers new insights into disease pathogenesis and paves the way for personalized medicine approaches.
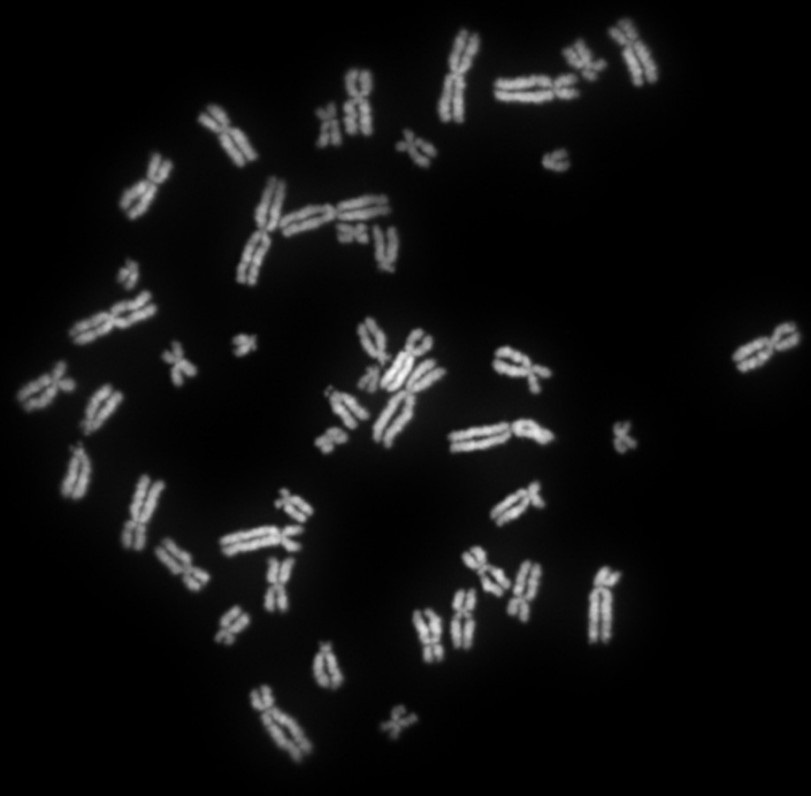
The female body’s handling of the additional X chromosome, a characteristic feature of biological sex determination in mammals, may play a crucial role in autoimmune susceptibility. Unlike males who possess one X chromosome paired with a shorter Y chromosome, females carry two X chromosomes in each cell. While the X chromosome harbors numerous genes vital for life, the presence of two X chromosomes increases the risk of overproduction of certain proteins, potentially leading to lethal outcomes. To counteract this risk, the female body employs a mechanism to deactivate one of the X chromosomes.
Central to this process is a specialized RNA molecule called Xist, which is produced by the surplus X chromosome in females. Xist binds to extensive regions of the additional X chromosome, effectively silencing its genetic activity while allowing the other X chromosome to function normally. However, this silencing mechanism inadvertently attracts a multitude of proteins, many of which have been implicated in autoimmune disorders.
Researchers hypothesized that the protein clusters formed as a result of X chromosome deactivation might contribute to the development of autoimmune diseases in women. To investigate this theory, scientists inserted the Xist gene into male laboratory mice predisposed to a lupus-like autoimmune condition. By activating and deactivating the Xist gene as needed, researchers observed the formation of protein clusters in male mice, mirroring the process seen in females.
Furthermore, male mice with an active Xist gene displayed an increased susceptibility to developing the lupus-like disorder when exposed to an irritant known to induce autoimmune reactions. This finding suggests that while Xist-associated protein clusters may heighten autoimmune risk, additional environmental triggers are required to initiate the disease process fully. Notably, not all female or Xist-activated male mice developed the autoimmune disorder, indicating the involvement of other genetic factors in disease manifestation.
The identification of Xist-linked protein clusters as potential biomarkers for autoimmune susceptibility offers promising avenues for diagnostic and therapeutic advancements. By analyzing blood samples from patients with autoimmune disorders, researchers identified specific autoantibodies targeting the proteins associated with Xist clusters. This discovery opens the door to the development of diagnostic tests capable of assessing an individual’s vulnerability to autoimmune diseases.
However, the journey to understanding the role of Xist in autoimmune disorders has been hindered by gender bias in medical research. Traditional approaches utilizing male cell lines as the standard reference have overlooked the significance of Xist and its associated protein complexes, particularly in assessing autoimmune susceptibility in women. Overcoming these biases is critical for advancing our understanding of autoimmune diseases and developing more effective treatments tailored to individual patient needs.
The elucidation of Xist-associated mechanisms sheds light on the complex relationship between gender, genetics, and autoimmune susceptibility. By identifying biomarkers and understanding the role of environmental triggers, researchers are poised to revolutionize the diagnosis and treatment of autoimmune disorders. Overcoming gender biases in medical research is crucial for harnessing these discoveries to improve outcomes for individuals affected by autoimmune diseases, ushering in a new era of precision medicine.
