Researchers in the UK have achieved a breakthrough in prenatal medicine by cultivating miniature organs from fetal cells found in amniotic fluid. These organoids offer a novel platform for studying fetal development, diagnosing congenital conditions, and developing personalized therapies. The innovative approach sidesteps ethical concerns associated with fetal tissue collection and extends opportunities for prenatal intervention. While further research is needed, this pioneering technique holds immense promise for revolutionizing prenatal care and improving outcomes for both mother and child.
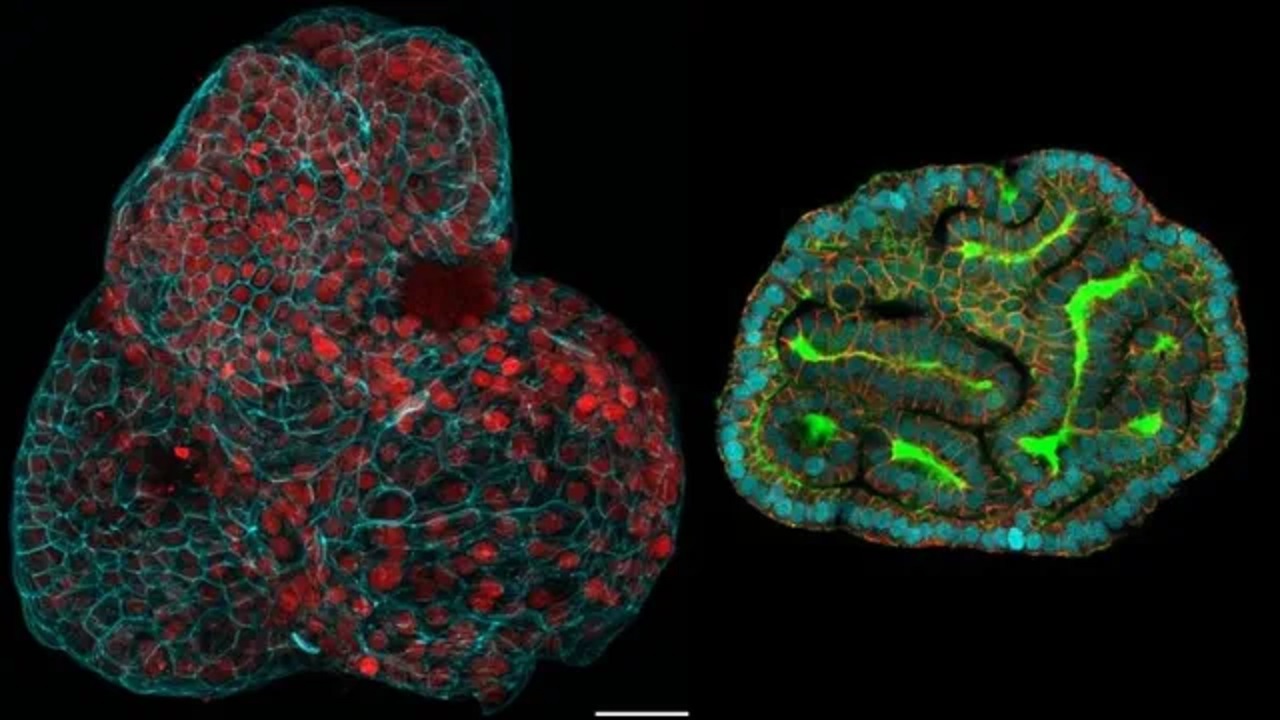
Researchers in the United Kingdom have achieved a groundbreaking feat by generating miniature organs from cells found in the fluid surrounding fetuses in the womb, offering a promising avenue for prenatal medicine. These miniature organs, known as organoids, represent simplified structures that can be utilized for testing novel medical interventions and exploring the functionality of real organs in both healthy and diseased states.
The pioneering work involved the collection of cells from amniotic fluid samples taken during 12 pregnancies as part of standard prenatal screening procedures. This marked the first instance of growing organoids from cells obtained during ongoing pregnancies. This innovative approach holds the potential to revolutionize prenatal care by facilitating the monitoring and treatment of congenital conditions before birth, as well as enabling the development of personalized therapies tailored to individual fetuses.
Lead researcher Mattia Gerli, affiliated with University College London, expressed excitement about the prospective applications of this breakthrough. The stem cells specific to various tissues were harvested from the fetus, a process that occurs naturally during pregnancy. These stem cells were identified to originate from organs such as the lungs, kidneys, and intestines.
Traditionally, organoids have been derived from adult stem cells or fetal tissue obtained after abortions. However, harvesting cells from amniotic fluid circumvents regulatory constraints associated with directly obtaining stem cells from fetal tissue. This method extends the window for collecting fetal cells beyond the legal limits for terminating pregnancies, thereby enhancing opportunities to investigate normal human development and congenital diseases during later stages of gestation.
In comparison to the United States, where regulations on abortion vary by state, the UK’s approach to obtaining fetal tissue for research purposes offers a more ethically acceptable alternative. According to Alta Charo, a professor of law and bioethics at the University of Wisconsin-Madison, collecting cells from amniotic fluid for clinical purposes poses no additional physical risks to the fetus or the pregnant woman.
Dr. Arnold Kriegstein, from the University of California, San Francisco, emphasized the potential of this method to provide insights into the development of individual fetuses. Given that the process of growing mini-organs from amniotic fluid cells takes several weeks, there is ample time for prenatal interventions to address any identified issues.
To demonstrate the practical utility of their approach, the UK-based research team collaborated with counterparts in Belgium to investigate congenital diaphragmatic hernia (CDH), a condition characterized by the displacement of abdominal organs into the chest cavity due to a hole in the diaphragm. This defect impedes proper lung development, resulting in a high mortality rate among affected fetuses. By growing lung organoids from cells obtained from both healthy fetuses and those with CDH, the researchers were able to assess the condition of affected fetuses before birth. This represents a significant advancement in prenatal diagnostics and holds promise for enhancing prognostic accuracy and treatment efficacy.
Dr. Paolo de Coppi, a co-author of the study, underscored the significance of studying functional prenatal organoids as a critical step toward improving prognostic capabilities and treatment outcomes for congenital conditions. However, Dr. Kriegstein cautioned that further research is necessary to fully evaluate the clinical utility of this approach, acknowledging that it is still in its early stages.
The cultivation of mini-organs from fetal cells obtained from amniotic fluid marks a transformative milestone in prenatal medicine. This innovative technique not only provides insights into fetal development but also holds promise for enhancing prenatal diagnostics and personalized therapeutic interventions. While further research is necessary to fully realize its clinical potential, the implications of this advancement for improving prenatal care are profound. By leveraging the unique properties of fetal fluid cells, scientists are paving the way for a future where congenital conditions can be detected and treated more effectively, ultimately improving outcomes for both mother and child.
