Retraction of studies on mifepristone’s risks underscores the complexities of reproductive healthcare research. Flaws and conflicts of interest led to retractions, prompting scrutiny of legal rulings and potential impacts on medication abortion access. Despite controversy, experts affirm the safety and efficacy of medication abortions, emphasizing the need for evidence-based policymaking. Transparent research practices and unbiased peer review are essential to navigate contentious issues like reproductive healthcare.
Recently, a significant development has emerged in the realm of reproductive healthcare, as two studies shedding light on the alleged risks associated with the abortion pill mifepristone have been retracted by the medical journal Sage Perspectives. The retractions were prompted by identified flaws in the research methodologies and conflicts of interest associated with the authors.
These studies, published in the journal Health Services Research and Managerial Epidemiology, had been referenced in a pivotal Texas court ruling, potentially influencing access to medication abortion across the United States. With the U.S. Supreme Court set to deliberate on the case soon, the outcome could significantly impact the availability of mifepristone, including its accessibility via mail order—a crucial aspect of reproductive healthcare.
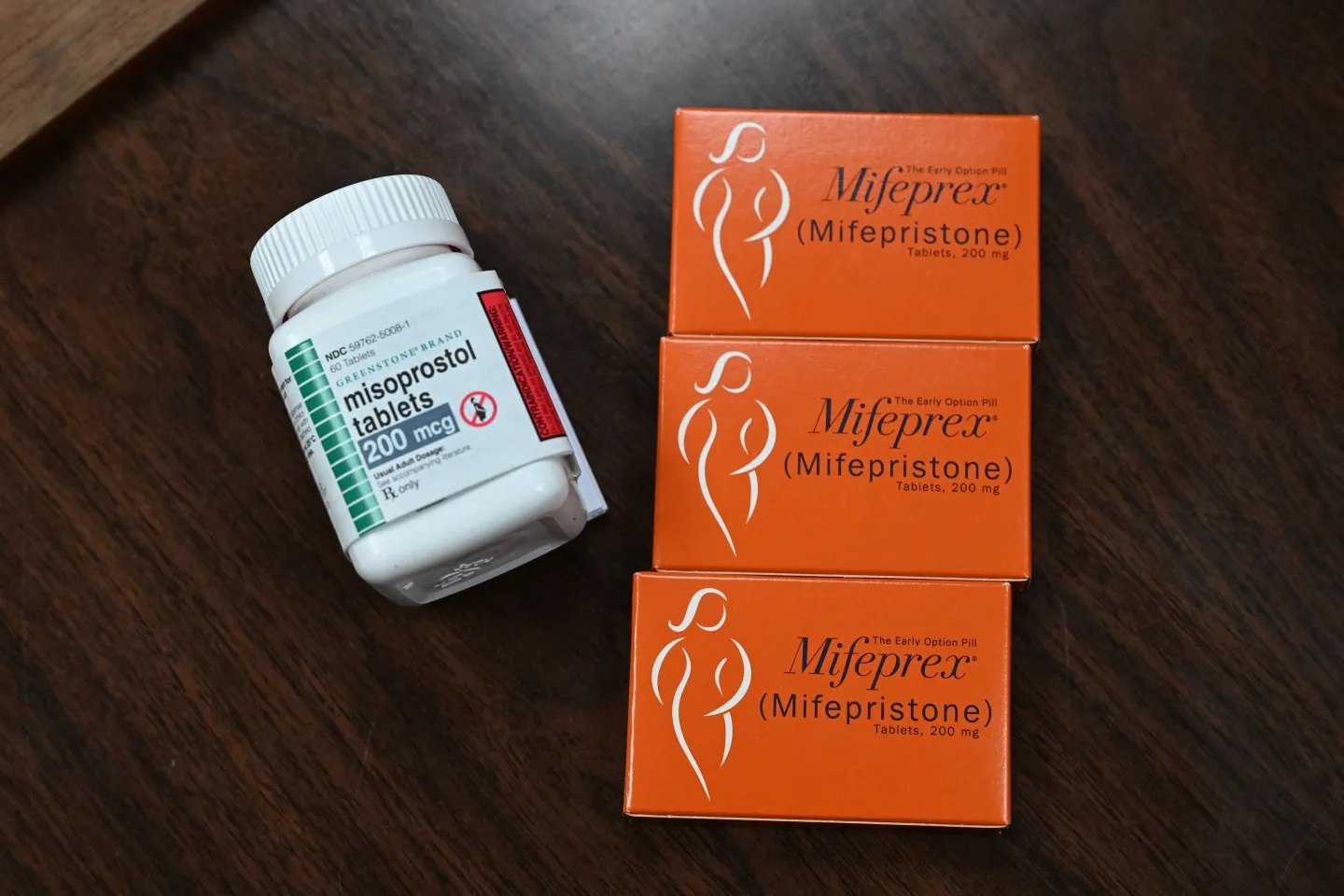
Mifepristone, often used in combination with misoprostol, constitutes a substantial portion of medication abortions in the U.S. Medication abortion, a safe and common procedure, plays a vital role in reproductive healthcare, comprising over half of all abortions in the country.
Understanding the Retractions: What Did the Studies Propose?
The retracted studies, both supported by the Charlotte Lozier Institute—an organization advocating against abortion—suggested an association between mifepristone usage and heightened risks of postabortion emergency room visits. One study analyzed a significant dataset spanning from 1999 to 2015, concluding that medication abortions were consistently linked with more postabortion ER visits compared to other methods.
Another study asserted that failure to disclose previous abortions during an ER visit posed a substantial risk factor for subsequent hospital admissions. These findings were instrumental in a legal ruling by U.S. District Judge Matthew Kacsmaryk, who contended that the original approval of mifepristone was flawed, citing safety concerns highlighted in the retracted studies.
Critique of the Studies and Legal Ramifications:
Kacsmaryk’s decision, heavily reliant on these studies, fueled a contentious legal battle that now stands before the highest court in the nation. However, skepticism regarding the studies’ validity emerged among legal experts and medical professionals, prompting a federal appeals court to overturn parts of the ruling.
The retraction stemmed from concerns raised about data presentation, methodological flaws, and potential conflicts of interest associated with the authors’ affiliations. Sage Perspectives initiated an independent peer review, which identified various shortcomings in the studies’ design, methodology, and data analysis.
James Studnicki, the lead author of the retracted studies and a vice president at the Charlotte Lozier Institute, dismissed the retractions as an unwarranted assault on their scientific research. Nonetheless, the retractions underscore the importance of rigorous research practices and transparent disclosure of affiliations in academic endeavors, particularly in contentious fields like reproductive healthcare.
Implications for Mifepristone Access and Reproductive Health:
While the retractions cast doubt on the studies’ findings, they do not directly challenge the FDA’s original approval of mifepristone. However, the Supreme Court’s decision could potentially roll back recent regulatory changes aimed at enhancing access to the drug, including its distribution via mail order—a development with significant ramifications for reproductive healthcare access nationwide.
In contrast to the studies’ assertions, experts emphasize the safety and efficacy of medication abortions, citing a low incidence of serious adverse events. Ushma Upadhyay, a professor at the University of California, San Francisco, underscores the extensive usage of mifepristone over the past two decades and its established safety profile.
Moreover, criticisms of the retracted research highlight the conflation of emergency room visits with serious adverse events, neglecting to verify whether patients received necessary treatment—a crucial aspect in assessing the actual risks associated with medication abortion.
Moving Forward: Ensuring Informed Policy and Healthcare Practices
As the legal and medical communities navigate this complex terrain, ensuring evidence-based policymaking and healthcare practices remains paramount. Transparent and unbiased research methodologies, coupled with robust peer review processes, are essential in guiding informed decision-making, particularly concerning sensitive issues like reproductive healthcare.
The retractions of studies on mifepristone’s risks highlight the intricate intersection of science, ideology, and policymaking in reproductive healthcare. Despite challenges to the validity of these studies, experts reaffirm the safety and importance of medication abortions in ensuring reproductive autonomy. Moving forward, upholding scientific integrity, transparent research practices, and evidence-based policymaking are essential to navigating the complexities of reproductive health, and safeguarding access to comprehensive and equitable care for all individuals.
